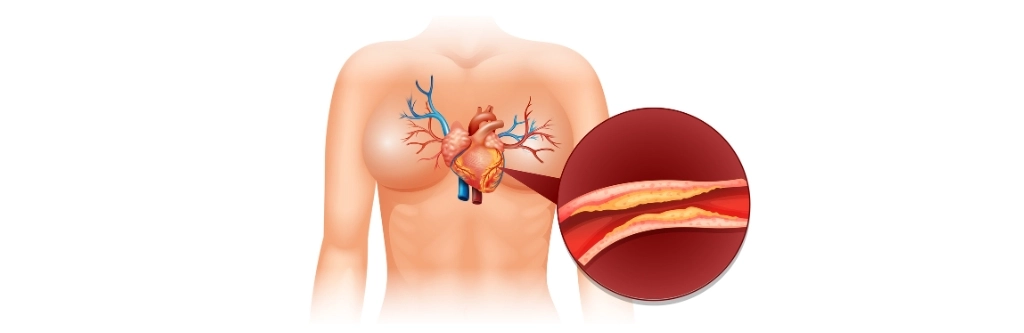
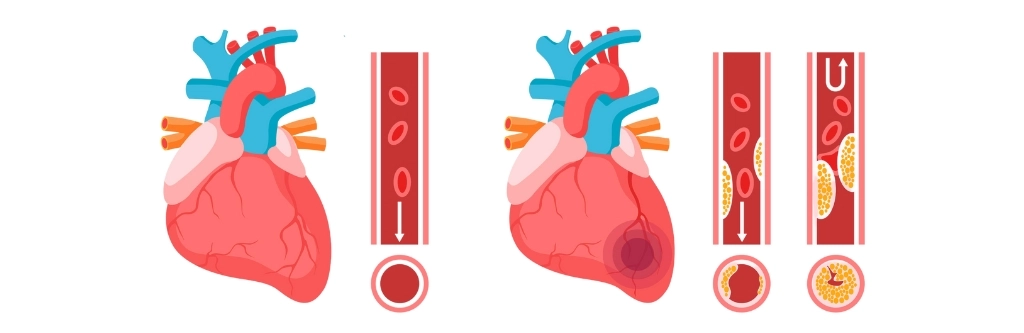
 Coronary Artery Disease (CAD) is a serious and prevalent condition that occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque. This plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. The reduction in blood flow can significantly impair the heart’s ability to receive adequate oxygen and nutrients, leading to a range of symptoms and complications.
Coronary Artery Disease (CAD) is a serious and prevalent condition that occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque. This plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. The reduction in blood flow can significantly impair the heart’s ability to receive adequate oxygen and nutrients, leading to a range of symptoms and complications.
The primary symptom of CAD is angina, or chest pain, which may feel like pressure, squeezing, or fullness in the chest. This pain can radiate to the arms, neck, jaw, or back. Additionally, individuals with CAD may experience shortness of breath, fatigue, or arrhythmias (irregular heartbeats). If left untreated, CAD can lead to more severe outcomes such as myocardial infarction (heart attack), heart failure, or even sudden cardiac death.
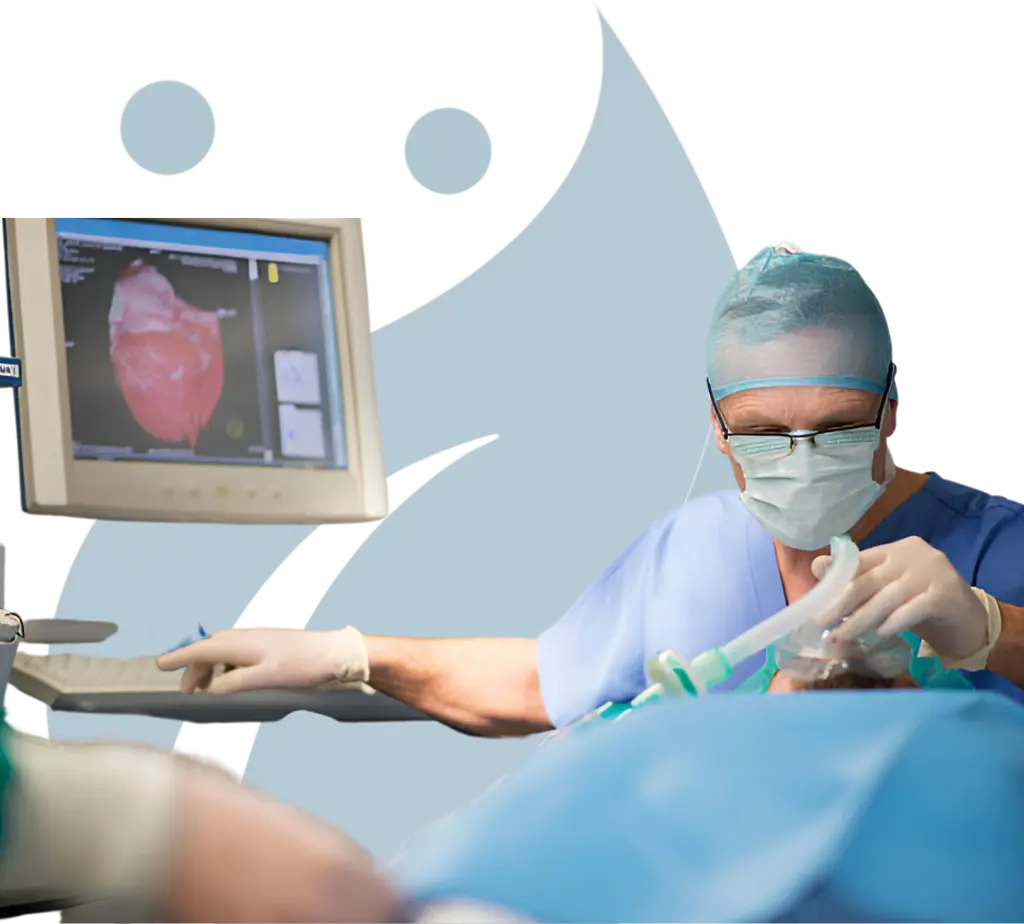
Given the critical nature of this condition, it is essential to provide precise anesthetic management during any surgical procedures. This involves careful monitoring and control of the patient’s hemodynamic status to ensure that the heart continues to function properly throughout the operation. Anesthesiologists play a vital role in managing CAD patients by optimizing oxygen delivery, minimizing stress on the heart, and preventing perioperative complications. Consulting with a cardiac anaesthesiologist in Chennai ensures expert care and tailored anesthesia management for CAD patients.
Treatments
- CABG Surgery: Coronary Artery Bypass Grafting (CABG) is a surgical procedure designed to restore adequate blood flow to the heart muscle by bypassing the blocked or narrowed coronary arteries. During CABG, a surgeon uses a healthy blood vessel from another part of the body, such as the leg, arm, or chest, to create a new pathway for blood to flow to the heart. This procedure is often recommended for patients with multiple blocked arteries or those who have not responded well to other treatments like angioplasty or medication. CABG has been shown to significantly improve symptoms, reduce the risk of heart attack, and increase survival rates in patients with severe CAD.
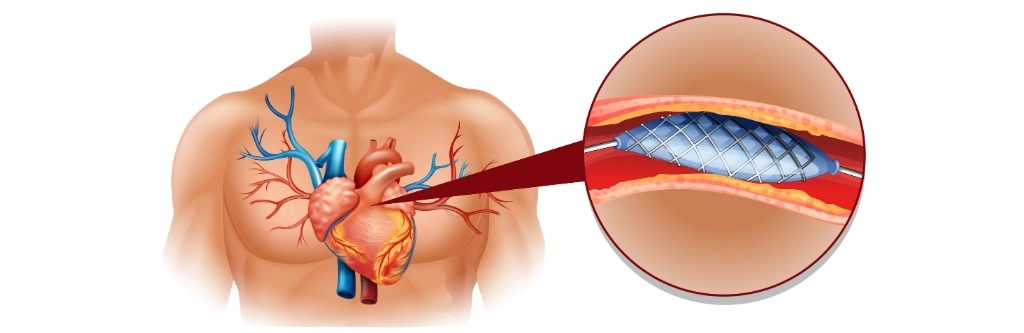
- Angioplasty: Angioplasty, also known as percutaneous coronary intervention (PCI), is a minimally invasive procedure used to open up narrowed or blocked coronary arteries. During angioplasty, a catheter with a small balloon at its tip is inserted into the narrowed artery. The balloon is then inflated, compressing the plaque against the artery walls and widening the artery to restore blood flow. Angioplasty is often performed in conjunction with stent placement to ensure that the artery remains open after the procedure. This treatment is particularly beneficial for patients with single-vessel disease or those who are not candidates for CABG surgery.
- Stent Placement: Stent placement is a common adjunct to angioplasty, where a small, mesh-like tube called a stent is inserted into the artery after it has been widened by the balloon. The stent acts as a scaffold, keeping the artery open and preventing it from narrowing again. There are two main types of stents: bare-metal stents and drug-eluting stents. Drug-eluting stents are coated with medication that helps prevent the re-narrowing of the artery, a condition known as restenosis. Stent placement has become a standard treatment for CAD, offering patients a less invasive alternative to surgery with quicker recovery times.
- Lifestyle Changes: Long-term management of CAD requires a comprehensive approach that includes significant lifestyle changes. Patients are encouraged to adopt a heart-healthy diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, while reducing the intake of saturated fats, cholesterol, and sodium. Regular physical activity, such as walking, swimming, or cycling, is also crucial for maintaining cardiovascular health. Additionally, quitting smoking, managing stress, and controlling conditions like hypertension, diabetes, and high cholesterol are vital steps in preventing the progression of CAD and improving overall heart health. Lifestyle changes are not only preventive but also help in the long-term management of CAD, reducing the risk of future cardiac events.
- Medication Management: Effective medication management is essential for controlling the symptoms of CAD and preventing complications such as heart attack or stroke. A variety of medications may be prescribed depending on the severity and specifics of the condition. These may include antiplatelet agents like aspirin, which help prevent blood clots; statins, which lower cholesterol levels; beta-blockers and ACE inhibitors, which reduce the heart’s workload; and nitrates, which relieve chest pain. In some cases, anticoagulants, calcium channel blockers, or newer medications like PCSK9 inhibitors may be used. Regular follow-up with the best cardiac anesthesia specialist in Chennai is crucial to adjust medications as needed and to monitor for any side effects or interactions.
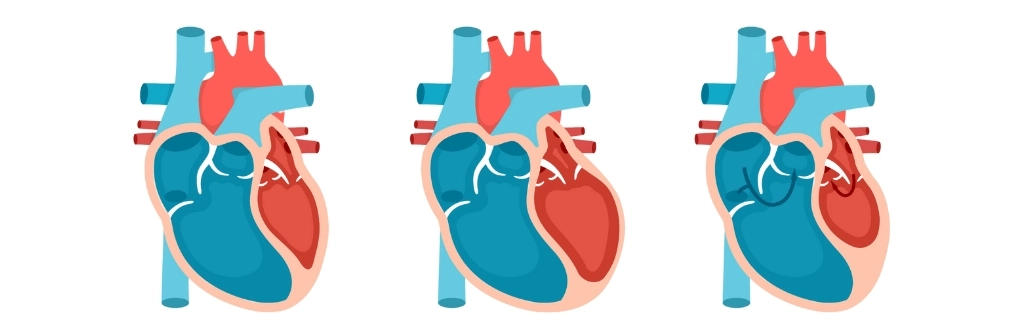
 Valvular Heart Disease is a condition that impairs the function of one or more of the heart’s valves, which play a critical role in ensuring unidirectional blood flow through the heart chambers. These valves include the mitral, aortic, tricuspid, and pulmonary valves. When any of these valves are damaged or malfunctioning, it can lead to significant complications, such as regurgitation (where the blood flows backward due to improper valve closure) or stenosis (where the valve narrows, restricting blood flow).
Valvular Heart Disease is a condition that impairs the function of one or more of the heart’s valves, which play a critical role in ensuring unidirectional blood flow through the heart chambers. These valves include the mitral, aortic, tricuspid, and pulmonary valves. When any of these valves are damaged or malfunctioning, it can lead to significant complications, such as regurgitation (where the blood flows backward due to improper valve closure) or stenosis (where the valve narrows, restricting blood flow).
Both conditions place additional strain on the heart, leading to decreased cardiac efficiency, increased workload, and potentially heart failure if left untreated. Early diagnosis and appropriate management are crucial for preserving heart function and quality of life. For comprehensive care, including surgical interventions, consulting with the top cardiac anaesthesiologist for heart in Chennai can provide specialized expertise in managing these complex conditions.
Treatments
- Valve Repair: Valve repair is a surgical procedure aimed at fixing the damaged valve to restore its normal function. This is often the preferred treatment when the valve’s structure is still largely intact, allowing the surgeon to correct specific issues such as leaflet thickening or tearing. Repairing the valve instead of replacing it can help maintain the natural heart function, reduce the need for lifelong medication, and lower the risk of infection and blood clots.
- Valve Replacement: When a heart valve is too damaged to be repaired, valve replacement becomes necessary. This procedure involves removing the malfunctioning valve and replacing it with a prosthetic one, which can be either mechanical or biological. Mechanical valves are durable and last longer but require lifelong blood-thinning medication. Biological valves, typically made from animal tissue, may not last as long but generally do not require long-term anticoagulation. The choice between repair and replacement depends on factors such as the valve’s condition, the patient’s overall health, and the potential for long-term success.
- Balloon Valvuloplasty: Balloon Valvuloplasty is a minimally invasive procedure used primarily for treating stenotic valves, especially in patients who may not be ideal candidates for open-heart surgery. In this procedure, a balloon-tipped catheter is threaded through the blood vessels to the narrowed valve. Once in position, the balloon is inflated, which helps to widen the valve opening and improve blood flow. While this procedure can be highly effective, it may not be a permanent solution, and some patients may eventually require valve replacement.
- Medication: Medication plays a crucial role in managing the symptoms of Valvular Heart Disease and preventing further complications. Depending on the specific condition, medications may include diuretics to reduce fluid buildup, beta-blockers to manage heart rate and blood pressure, and anticoagulants to prevent blood clots. In some cases, medications may help manage the condition long-term or serve as a bridge to surgery, but they are not typically a cure for valve disease.
- Endocarditis Prevention: Patients with Valvular Heart Disease are at increased risk of developing endocarditis, an infection of the heart valves. This can occur when bacteria enter the bloodstream and attach to the damaged valve tissue. Preventive measures include maintaining good oral hygiene, as dental procedures can introduce bacteria into the bloodstream, and taking antibiotics before certain medical or dental procedures if recommended by a healthcare provider. Proper management and prevention of endocarditis are vital for protecting vulnerable heart valves and ensuring long-term heart health.
For comprehensive care and advanced treatment options, consulting with a cardiac anaesthesiologist in Chennai can enhance the management of Valvular Heart Disease, ensuring optimal surgical outcomes and overall heart health.
 Arrhythmias are irregular heartbeats that can significantly impact the heart’s ability to pump blood effectively, potentially leading to serious complications such as stroke, heart failure, or sudden cardiac arrest. These irregularities in the heart’s rhythm may be caused by various factors, including structural abnormalities of the heart, electrolyte imbalances, or damage to the heart tissue. During surgeries, particularly those involving the heart or major blood vessels, maintaining a stable heart rhythm is of utmost importance to prevent life-threatening events. This requires the implementation of tailored anesthetic strategies designed to minimize the risk of exacerbating the arrhythmia or triggering new irregularities.
Arrhythmias are irregular heartbeats that can significantly impact the heart’s ability to pump blood effectively, potentially leading to serious complications such as stroke, heart failure, or sudden cardiac arrest. These irregularities in the heart’s rhythm may be caused by various factors, including structural abnormalities of the heart, electrolyte imbalances, or damage to the heart tissue. During surgeries, particularly those involving the heart or major blood vessels, maintaining a stable heart rhythm is of utmost importance to prevent life-threatening events. This requires the implementation of tailored anesthetic strategies designed to minimize the risk of exacerbating the arrhythmia or triggering new irregularities.
Treatments
- Electrophysiology Study (EPS): The electrophysiology study is a diagnostic procedure used to determine the type and origin of arrhythmias. During an EPS, catheters equipped with electrodes are inserted into the heart through blood vessels to map the electrical signals within the heart. This detailed mapping allows the cardiologist to pinpoint the exact location of the abnormal electrical activity, which is essential for planning further treatment, such as catheter ablation or pacemaker implantation.
- Catheter Ablation: Catheter ablation is a minimally invasive procedure aimed at treating arrhythmias by destroying the small areas of heart tissue that are responsible for the abnormal electrical signals. During the procedure, a catheter is guided through the blood vessels to the heart, where it delivers energy (such as radiofrequency or cryoenergy) to the targeted tissue, thereby eliminating the source of the arrhythmia. This procedure is highly effective for certain types of arrhythmias, such as atrial fibrillation or ventricular tachycardia, and can significantly reduce or eliminate the need for ongoing medication.
- Pacemaker Implantation: Pacemaker implantation involves placing a small electronic device under the skin near the heart to regulate the heart’s rhythm. The pacemaker monitors the heart’s electrical activity and, when necessary, sends electrical impulses to stimulate the heart to beat at a normal rate. Pacemakers are particularly useful for treating slow heart rhythms (bradycardia) or for patients who have experienced heart block. The device is usually implanted during a minor surgical procedure and can significantly improve the quality of life for individuals with certain arrhythmias.
- Medication: Medications play a crucial role in the management of arrhythmias. Antiarrhythmic drugs are used to control heart rate and rhythm, preventing the occurrence of arrhythmias or reducing their severity. These medications may be prescribed for long-term use or as a temporary measure until more definitive treatments, such as catheter ablation, can be performed. The choice of medication depends on the specific type of arrhythmia, the patient’s overall health, and other underlying conditions.
- Lifestyle Modifications: Lifestyle modifications are an essential component of managing arrhythmias, as certain habits and conditions can trigger or worsen irregular heartbeats. Patients are often advised to adopt a heart-healthy diet, engage in regular physical activity, avoid excessive alcohol and caffeine intake, and manage stress effectively. Additionally, quitting smoking and maintaining a healthy weight can reduce the frequency and severity of arrhythmias. These lifestyle changes not only help control arrhythmias but also contribute to overall cardiovascular health, reducing the risk of other heart-related complications.
For expert care in managing arrhythmias, consulting with a cardiac anaesthesiologist in Chennai can ensure a comprehensive approach to treatment and anesthesia during cardiac procedures.
 Heart failure is a chronic and progressive condition where the heart’s ability to pump blood efficiently is compromised. This results in the body’s organs and tissues receiving insufficient oxygen and nutrients, leading to symptoms such as persistent fatigue, swelling in the legs, ankles, or abdomen (edema), and significant difficulty in breathing, especially during physical exertion or while lying down. As the heart struggles to meet the body’s demands, patients may experience a decrease in exercise tolerance, frequent coughing or wheezing, and rapid or irregular heartbeats.
Heart failure is a chronic and progressive condition where the heart’s ability to pump blood efficiently is compromised. This results in the body’s organs and tissues receiving insufficient oxygen and nutrients, leading to symptoms such as persistent fatigue, swelling in the legs, ankles, or abdomen (edema), and significant difficulty in breathing, especially during physical exertion or while lying down. As the heart struggles to meet the body’s demands, patients may experience a decrease in exercise tolerance, frequent coughing or wheezing, and rapid or irregular heartbeats.
Treatments
- Medication Management: Managing heart failure often begins with medications aimed at improving heart function, reducing symptoms, and preventing further damage. Common medications include ACE inhibitors, which help relax blood vessels and lower blood pressure, beta-blockers that reduce the heart rate and decrease its workload, and diuretics to help the body eliminate excess fluid. The precise combination of drugs is tailored to each patient’s specific condition, helping to control symptoms and slow the progression of the disease.
- Implantable Devices: For patients with severe heart failure, implantable devices can play a crucial role in supporting heart function. Left Ventricular Assist Devices (LVADs), for instance, are mechanical pumps that help the left ventricle pump blood to the rest of the body, offering a lifeline for those awaiting heart transplants or those who are not candidates for surgery. Implantable cardioverter-defibrillators (ICDs) are another option, used to prevent sudden cardiac death by correcting life-threatening arrhythmias.
- Cardiac Resynchronization Therapy (CRT): Cardiac Resynchronization Therapy is a specialized treatment that helps improve the efficiency of the heart by coordinating the timing of the heart’s contractions. In heart failure patients, the ventricles may not beat in sync, reducing the heart’s efficiency. CRT uses a device similar to a pacemaker to send electrical impulses to the heart’s ventricles, ensuring that they contract simultaneously, which can significantly enhance the heart’s ability to pump blood and improve the patient’s quality of life.
- Surgical Repair: In cases where heart failure is caused by structural heart problems, such as valve disorders or congenital heart defects, surgical intervention may be necessary. Procedures like valve repair or replacement, coronary artery bypass grafting (CABG), or the correction of congenital defects can address the underlying causes of heart failure, potentially improving heart function and alleviating symptoms. Surgical repair often provides significant relief, although it requires careful consideration of the patient’s overall health and the risks associated with surgery.
- Diet and Exercise: Long-term management of heart failure is heavily dependent on lifestyle changes, particularly diet and exercise. A heart-healthy diet low in sodium and rich in fruits, vegetables, whole grains, and lean proteins helps reduce fluid retention and blood pressure, easing the strain on the heart. Regular, moderate exercise tailored to the patient’s abilities can strengthen the heart muscle, improve circulation, and enhance overall endurance. Together, these lifestyle modifications are essential components of a comprehensive heart failure management plan, helping to control symptoms, improve quality of life, and prevent the progression of the disease.
For comprehensive care, including surgical procedures and anesthesia management, consulting a cardiac anaesthesiologist in Chennai can ensure expert handling of complex cases and optimal patient outcomes.
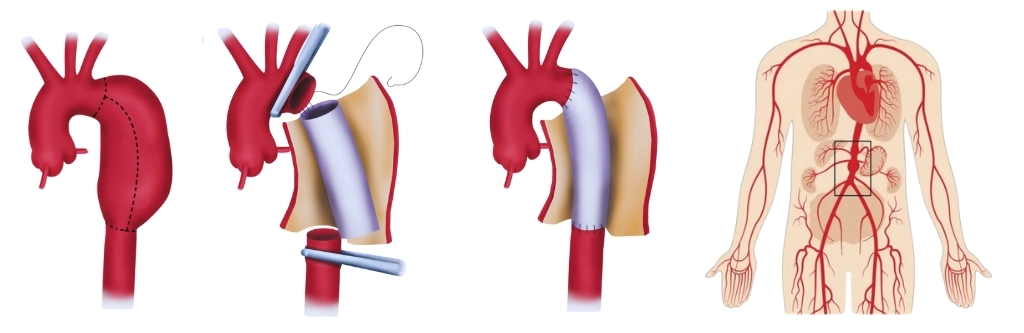 An Aortic Aneurysm is a serious medical condition characterized by a localized enlargement or bulging of the aorta, the largest artery in the body. This bulging occurs due to a weakened area in the arterial wall, which can lead to the vessel’s dilation. Over time, the aneurysm can grow larger, increasing the risk of rupture. A ruptured Aortic Aneurysm is a medical emergency as it can cause life-threatening internal bleeding, leading to shock or even death if not treated promptly.
An Aortic Aneurysm is a serious medical condition characterized by a localized enlargement or bulging of the aorta, the largest artery in the body. This bulging occurs due to a weakened area in the arterial wall, which can lead to the vessel’s dilation. Over time, the aneurysm can grow larger, increasing the risk of rupture. A ruptured Aortic Aneurysm is a medical emergency as it can cause life-threatening internal bleeding, leading to shock or even death if not treated promptly.
The condition requires immediate and precise medical intervention, often involving a multidisciplinary team of surgeons, anesthesiologists, and other specialists. Proper anesthetic management during surgical repair is crucial to minimizing complications, such as bleeding, stroke, or organ failure. For expert anesthetic care, consulting a cardiac anaesthesiologist in Chennai can ensure optimal outcomes during the surgical procedure.
Treatments
- Open Aneurysm Repair: Open Aneurysm Repair is a traditional surgical method where the surgeon makes a large incision in the abdomen or chest to access the aorta. The damaged section of the aorta is surgically removed and replaced with a synthetic graft made of materials like Dacron or Teflon. This procedure is highly effective but involves significant recovery time due to the invasive nature of the surgery. Patients require general anaesthesia, and post-operative care includes intensive monitoring in a hospital setting to ensure proper healing and prevent complications such as infections or graft-related issues.
- Endovascular Repair: Endovascular Repair is a less invasive alternative to open surgery. This approach involves inserting a catheter through a small incision in the groin and guiding it to the site of the aneurysm. A stent graft is then deployed through the catheter to reinforce the weakened section of the aorta, preventing it from rupturing. This procedure typically results in shorter recovery times and fewer complications compared to open surgery. However, not all aneurysms are suitable for endovascular repair, and patients may require regular follow-up imaging to monitor the stent graft and ensure its continued effectiveness.
- Medication: Medications play a critical role in managing an Aortic Aneurysm, particularly in controlling the risk factors that can contribute to its growth. Blood pressure-lowering medications, such as beta-blockers and ACE inhibitors, are often prescribed to reduce the pressure on the aneurysm wall, thereby slowing its expansion. Additionally, statins may be used to manage cholesterol levels, further reducing the risk of aneurysm progression. While medication cannot repair the aneurysm, it is essential in preventing complications and preparing the patient for potential surgical intervention.
- Regular Monitoring: Regular monitoring is essential for patients diagnosed with an Aortic Aneurysm, especially if the aneurysm is small and does not require immediate surgery. This involves periodic imaging tests, such as ultrasound, CT scans, or MRI, to track the size and growth of the aneurysm. Monitoring helps healthcare providers assess the risk of rupture and determine the optimal timing for surgical intervention. Consistent follow-up is crucial in ensuring that any changes in the aneurysm’s size or shape are promptly addressed to prevent sudden complications.
- Lifestyle Changes: Lifestyle changes are a vital component of managing an Aortic Aneurysm. Patients are advised to adopt a heart-healthy lifestyle to reduce the risk of aneurysm growth and rupture. This includes quitting smoking, as smoking is a significant risk factor for aneurysm formation and progression. A balanced diet low in saturated fats and rich in fruits, vegetables, and whole grains can help manage cholesterol levels and blood pressure. Regular physical activity, tailored to the patient’s condition, also contributes to overall cardiovascular health. Additionally, managing stress through relaxation techniques and ensuring regular medical check-ups are essential in maintaining long-term health and preventing complications related to Aortic Aneurysms.
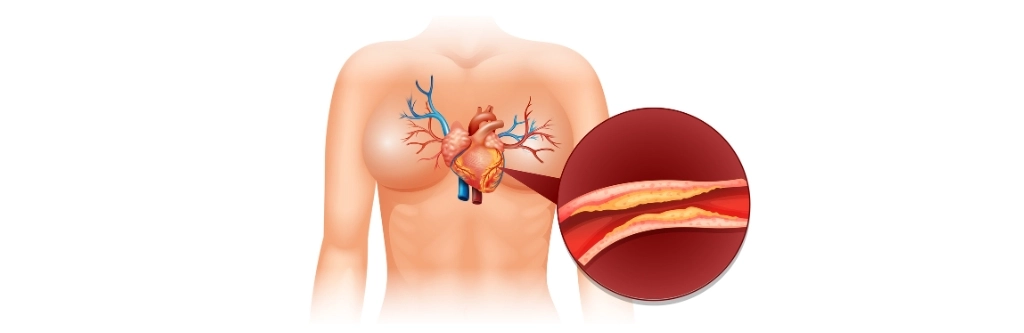 Coronary Artery Disease (CAD) is a serious and prevalent condition that occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque. This plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. The reduction in blood flow can significantly impair the heart’s ability to receive adequate oxygen and nutrients, leading to a range of symptoms and complications.
Coronary Artery Disease (CAD) is a serious and prevalent condition that occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque. This plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. The reduction in blood flow can significantly impair the heart’s ability to receive adequate oxygen and nutrients, leading to a range of symptoms and complications.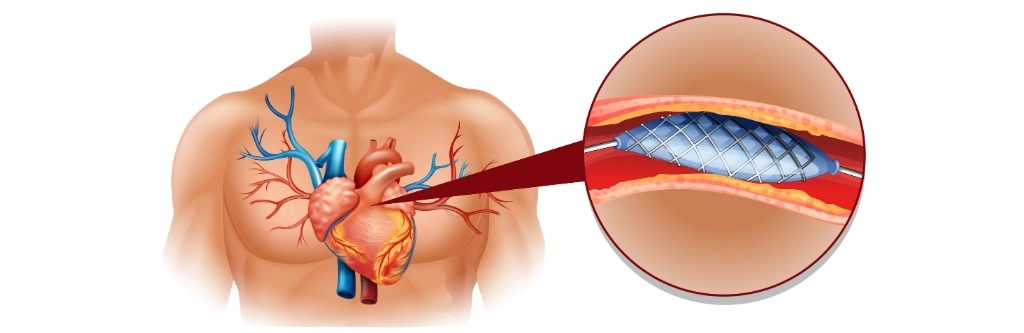 Valvular Heart Disease is a condition that impairs the function of one or more of the heart’s valves, which play a critical role in ensuring unidirectional blood flow through the heart chambers. These valves include the mitral, aortic, tricuspid, and pulmonary valves. When any of these valves are damaged or malfunctioning, it can lead to significant complications, such as regurgitation (where the blood flows backward due to improper valve closure) or stenosis (where the valve narrows, restricting blood flow).
Valvular Heart Disease is a condition that impairs the function of one or more of the heart’s valves, which play a critical role in ensuring unidirectional blood flow through the heart chambers. These valves include the mitral, aortic, tricuspid, and pulmonary valves. When any of these valves are damaged or malfunctioning, it can lead to significant complications, such as regurgitation (where the blood flows backward due to improper valve closure) or stenosis (where the valve narrows, restricting blood flow).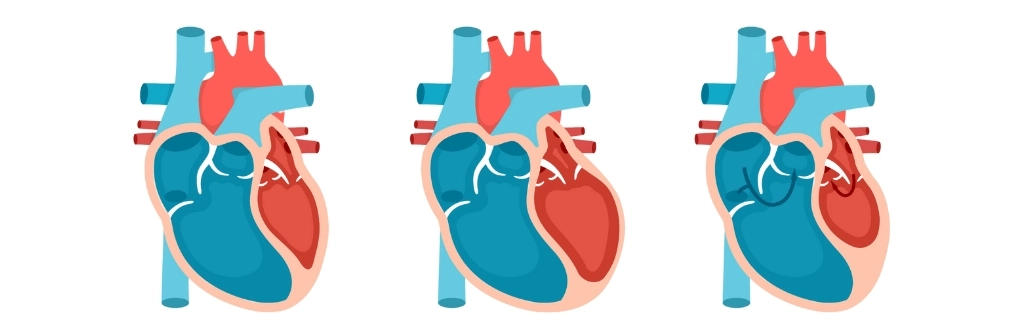 Arrhythmias are irregular heartbeats that can significantly impact the heart’s ability to pump blood effectively, potentially leading to serious complications such as stroke, heart failure, or sudden cardiac arrest. These irregularities in the heart’s rhythm may be caused by various factors, including structural abnormalities of the heart, electrolyte imbalances, or damage to the heart tissue. During surgeries, particularly those involving the heart or major blood vessels, maintaining a stable heart rhythm is of utmost importance to prevent life-threatening events. This requires the implementation of tailored anesthetic strategies designed to minimize the risk of exacerbating the arrhythmia or triggering new irregularities.
Arrhythmias are irregular heartbeats that can significantly impact the heart’s ability to pump blood effectively, potentially leading to serious complications such as stroke, heart failure, or sudden cardiac arrest. These irregularities in the heart’s rhythm may be caused by various factors, including structural abnormalities of the heart, electrolyte imbalances, or damage to the heart tissue. During surgeries, particularly those involving the heart or major blood vessels, maintaining a stable heart rhythm is of utmost importance to prevent life-threatening events. This requires the implementation of tailored anesthetic strategies designed to minimize the risk of exacerbating the arrhythmia or triggering new irregularities.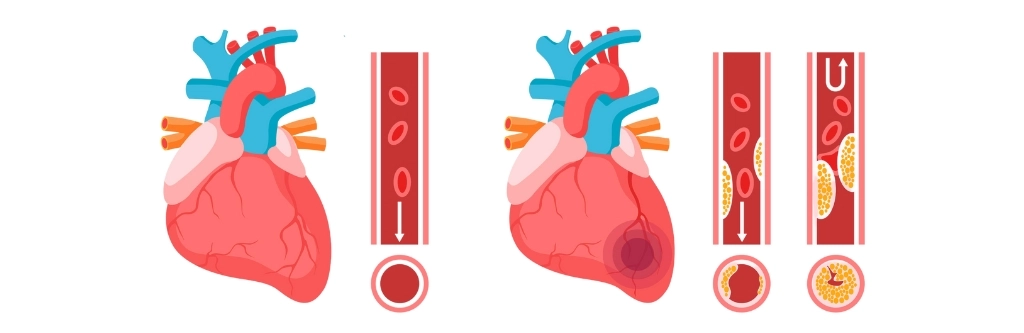 Heart failure is a chronic and progressive condition where the heart’s ability to pump blood efficiently is compromised. This results in the body’s organs and tissues receiving insufficient oxygen and nutrients, leading to symptoms such as persistent fatigue, swelling in the legs, ankles, or abdomen (edema), and significant difficulty in breathing, especially during physical exertion or while lying down. As the heart struggles to meet the body’s demands, patients may experience a decrease in exercise tolerance, frequent coughing or wheezing, and rapid or irregular heartbeats.
Heart failure is a chronic and progressive condition where the heart’s ability to pump blood efficiently is compromised. This results in the body’s organs and tissues receiving insufficient oxygen and nutrients, leading to symptoms such as persistent fatigue, swelling in the legs, ankles, or abdomen (edema), and significant difficulty in breathing, especially during physical exertion or while lying down. As the heart struggles to meet the body’s demands, patients may experience a decrease in exercise tolerance, frequent coughing or wheezing, and rapid or irregular heartbeats.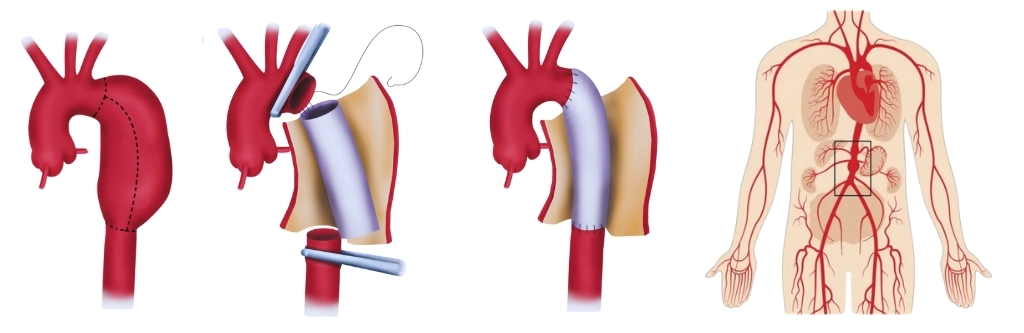 An Aortic Aneurysm is a serious medical condition characterized by a localized enlargement or bulging of the aorta, the largest artery in the body. This bulging occurs due to a weakened area in the arterial wall, which can lead to the vessel’s dilation. Over time, the aneurysm can grow larger, increasing the risk of rupture. A ruptured Aortic Aneurysm is a medical emergency as it can cause life-threatening internal bleeding, leading to shock or even death if not treated promptly.
An Aortic Aneurysm is a serious medical condition characterized by a localized enlargement or bulging of the aorta, the largest artery in the body. This bulging occurs due to a weakened area in the arterial wall, which can lead to the vessel’s dilation. Over time, the aneurysm can grow larger, increasing the risk of rupture. A ruptured Aortic Aneurysm is a medical emergency as it can cause life-threatening internal bleeding, leading to shock or even death if not treated promptly.